How I Finally Beat Stubborn Bloating—And Found Calm in the Process
Ever feel like your body’s holding onto more than just stress? For years, I struggled with occasional constipation and that heavy, bloated feeling that just wouldn’t quit. I tried quick fixes, but nothing lasted—until I realized my gut and mind were deeply connected. Turns out, calming the nervous system wasn’t just good for anxiety; it transformed my digestion. This is how small, science-backed shifts in daily rhythm made a real difference. What began as a search for digestive relief became a journey toward greater bodily awareness and emotional balance. The solution wasn’t found in a pill or a drastic cleanse, but in understanding the quiet signals my body had been sending all along.
The Hidden Link Between Stress and Digestion
The human body is not a collection of isolated systems—it functions as a deeply interconnected network, and nowhere is this more evident than in the relationship between the brain and the gut. Known as the gut-brain axis, this bidirectional communication pathway links emotional and cognitive centers in the brain with intestinal functions. When stress arises, whether from work pressure, personal responsibilities, or emotional strain, the nervous system shifts into a state of high alert—commonly referred to as the fight-or-flight response. In this mode, the body prioritizes survival over digestion. Blood flow is redirected away from the digestive organs, stomach acid production slows, and intestinal motility decreases. This physiological shift, while protective in acute danger, becomes problematic when activated chronically.
Over time, persistent stress can disrupt the natural rhythm of digestion, leading to symptoms like bloating, gas, and infrequent bowel movements. The digestive tract relies on a state of calm—known as the rest-and-digest mode—to function efficiently. This state is governed by the parasympathetic nervous system, which activates when the body feels safe and relaxed. When the nervous system remains in a heightened state, the gut struggles to perform its essential tasks, including breaking down food, absorbing nutrients, and eliminating waste. As a result, many people experience what feels like stubborn digestive issues, when in fact the root cause may be unresolved stress.
Consider the case of a woman in her early 40s, managing a demanding job while caring for two school-aged children. During high-pressure workweeks, she noticed a consistent pattern: her abdomen would swell uncomfortably by midday, she’d feel sluggish after meals, and bowel movements became irregular. Despite eating what she believed to be a healthy diet, relief was elusive. Only when she began tracking her symptoms alongside her stress levels did a pattern emerge—her worst digestive days coincided with her most emotionally taxing ones. This is not an isolated experience. Research has shown that individuals with higher perceived stress levels are more likely to report gastrointestinal discomfort, including bloating and constipation. The body, it seems, does not separate mental strain from physical sensation.
Why Quick Fixes Fail (And What Actually Works)
It’s natural to seek immediate relief when bloating or constipation strikes. Many turn to over-the-counter remedies such as stimulant laxatives, fiber supplements, or detox teas, hoping for a quick reset. While these solutions may provide temporary results, they often fail to address the underlying causes of digestive discomfort. Worse, they can create dependency or even worsen the problem over time. Stimulant laxatives, for example, work by irritating the lining of the intestines to force contractions. Regular use can lead the colon to become less responsive on its own, reducing natural motility and creating a cycle of reliance. Similarly, abruptly increasing fiber intake without adequate hydration can result in increased gas, abdominal distension, and even worsened constipation.
Another common pitfall is treating digestion as a purely mechanical issue—something to be fixed with a single supplement or dietary tweak—without considering the broader context of lifestyle and nervous system regulation. The digestive system is not a machine that can be forced into action; it is a living, responsive system influenced by sleep, movement, emotional state, and daily routines. Sustainable digestive health requires an approach that supports the body’s natural rhythms rather than overriding them. This means moving away from short-term interventions and toward consistent, body-friendly habits that nurture both gut function and overall well-being.
What actually works is a holistic, science-supported strategy that honors the body’s need for rhythm and regulation. This includes gentle hydration practices, mindful eating, consistent movement, and stress-reduction techniques—all of which help restore the conditions necessary for healthy digestion. Rather than forcing the body to comply, this approach invites it to return to balance. For instance, establishing a regular morning routine that includes water, light stretching, and deep breathing can signal to the body that it is safe to begin the day’s digestive processes. These small, daily actions build resilience over time, allowing the gut to regain its natural ability to function without external crutches.
Morning Rituals That Wake Up Your Gut—Naturally
One of the most effective ways to support digestive health is to start the day with intention. A simple, 10-minute morning routine can set the tone for improved gut function and greater overall vitality. The key lies in creating conditions that activate the parasympathetic nervous system—the state in which digestion thrives. Begin by drinking a glass of warm water as soon as you wake. This gentle act helps stimulate the gastrointestinal tract, encouraging the stomach to produce gastric juices and signaling the intestines to prepare for the day’s first meal. Adding a small squeeze of lemon can enhance this effect by mildly stimulating bile production, which aids in fat digestion, without causing irritation to the stomach lining.
Following hydration, incorporate a few minutes of gentle movement. This might include stretching in bed, a brief walk around the house, or a few slow spinal twists. These movements help awaken the muscles involved in digestion and improve circulation to the abdominal organs. Even minor physical activation can prompt the intestines to begin peristalsis—the wave-like contractions that move food through the digestive tract. For many, this early movement is enough to trigger the urge to use the bathroom, reinforcing the body’s natural morning elimination rhythm.
Completing the routine with mindful breathing further enhances its effectiveness. Diaphragmatic breathing—also known as belly breathing—engages the vagus nerve, a critical component of the parasympathetic nervous system. By taking slow, deep breaths that expand the lower abdomen, you send a signal to the brain that the body is safe and ready to digest. This practice not only calms the mind but also directly stimulates the enteric nervous system, often referred to as the “second brain” of the gut. Over time, consistent morning breathing exercises can improve bowel regularity and reduce bloating by fostering a state of internal calm. Together, these three elements—hydration, movement, and breath—form a powerful foundation for daily digestive wellness.
Movement as Medicine: Easy Daily Habits for Better Flow
Physical activity is one of the most accessible and effective tools for supporting healthy digestion. Movement encourages the muscles of the intestinal wall to contract, helping to propel contents through the digestive tract. This is particularly important for individuals who spend long hours sitting, as prolonged inactivity can slow transit time and contribute to feelings of fullness and bloating. The good news is that intense workouts are not required—light, consistent motion is often more beneficial than sporadic, high-effort exercise. The goal is not to burn calories, but to keep the body’s internal systems gently active throughout the day.
One of the simplest and most effective habits is walking after meals. A 10- to 15-minute stroll following breakfast, lunch, or dinner can significantly enhance gastric emptying and reduce post-meal discomfort. This practice has been supported by research showing that light physical activity after eating helps regulate blood sugar and improves digestive efficiency. For those with limited mobility or time, even standing up and shifting weight from foot to foot for a few minutes can make a difference. The key is to avoid lying down or sitting still immediately after eating, as this can delay digestion and increase the likelihood of bloating.
Yoga offers additional benefits through specific poses that massage the abdominal organs and relieve tension in the digestive tract. Poses such as knees-to-chest (Apanasana), seated forward bends, and gentle twists help stimulate intestinal movement and release trapped gas. These poses are accessible to most people, regardless of fitness level, and can be practiced for just a few minutes each day. Similarly, desk stretches—such as seated spinal twists or side bends—can be incorporated into a workday to prevent stagnation. The cumulative effect of these small movements is profound: they keep the digestive system engaged, reduce the buildup of pressure in the abdomen, and support overall comfort. Over time, regular movement becomes less of a chore and more of a natural rhythm, seamlessly woven into daily life.
Food Choices That Keep Things Moving—Without the Bloat
Diet plays a central role in digestive health, but the answer is not simply to eat more fiber. While fiber is essential for regular bowel movements, the type, timing, and manner of consumption matter greatly. Soluble fiber, found in foods like oats, apples, and chia seeds, absorbs water and forms a gel-like substance that softens stool and supports smooth transit. Insoluble fiber, present in whole grains, vegetables, and nuts, adds bulk to stool and helps it move more quickly through the colon. A balanced intake of both types is ideal, but it’s important to introduce fiber gradually to allow the gut microbiome to adapt. A sudden increase can overwhelm the digestive system, leading to gas, cramping, and increased bloating.
Some foods are particularly effective at promoting gentle movement. Prunes, for example, contain both fiber and sorbitol, a natural sugar alcohol that has a mild laxative effect. Chia seeds absorb many times their weight in water, forming a gel that aids in stool softening and regularity. Fermented foods like yogurt, kefir, and sauerkraut support a healthy gut microbiome, which plays a crucial role in digestion and immune function. However, not all high-fiber foods work for everyone. Some individuals may find that cruciferous vegetables, beans, or carbonated drinks trigger bloating due to their fermentable carbohydrate content. Identifying personal triggers through mindful eating and observation is key to building a diet that supports comfort and consistency.
Equally important is how food is consumed. Chewing thoroughly breaks down food into smaller particles, making it easier for the stomach and intestines to process. Eating too quickly or while distracted can lead to swallowing air and poor digestion, both of which contribute to bloating. Establishing regular meal times also supports digestive rhythm, as the body learns to anticipate and prepare for food intake. Hydration is another critical factor—without adequate water, fiber cannot do its job effectively. Stool becomes hard and difficult to pass, leading to discomfort and irregularity. Drinking water throughout the day, especially with meals and high-fiber foods, ensures that the digestive system has the fluid it needs to function smoothly.
Stress Signals Your Gut Is Sending (And How to Respond)
The gut is often called the “second brain” for good reason—it is lined with millions of neurons and is highly sensitive to emotional states. When stress builds, the gut is often the first place it shows up. Many people report feeling “butterflies” in their stomach before a big event, or a “knot” of tension during times of anxiety. For some, chronic stress manifests as persistent bloating, cramping, or changes in bowel habits. These are not imagined symptoms; they are real physiological responses to emotional strain. The gut communicates with the brain through neural, hormonal, and immune pathways, and when the mind is under pressure, the gut reflects that imbalance.
Learning to recognize these signals is the first step toward breaking the stress-digestion cycle. For instance, noticing that your abdomen tightens during a tense phone call or that bloating worsens on days when you feel overwhelmed can provide valuable insight. Once you become aware of these patterns, you can begin to intervene. Simple techniques like box breathing—inhaling for four counts, holding for four, exhaling for four, and pausing for four—can quickly shift the nervous system from fight-or-flight to rest-and-digest. This practice can be done anywhere and takes less than a minute, yet it has a measurable effect on reducing physiological stress.
Grounding exercises are another effective tool. Focusing on the sensation of your feet on the floor, naming five things you can see, or taking a few slow breaths while placing a hand on your abdomen can bring your attention back to the present moment and calm the nervous system. Short mindfulness breaks—pausing to check in with your body every few hours—help build long-term awareness. Over time, these practices train the body to respond to stress with greater resilience, reducing its impact on digestion. The goal is not to eliminate stress entirely—that is neither possible nor desirable—but to develop a healthier relationship with it, so it no longer disrupts your gut health.
Building a Lifestyle That Supports Regularity—From the Inside Out
Sustainable digestive wellness is not achieved through isolated fixes, but through the integration of small, consistent habits that align with the body’s natural rhythms. The most effective approach is one that combines hydration, movement, mindful eating, and nervous system regulation into a seamless daily routine. This doesn’t require drastic changes or hours of effort. Instead, it’s about making intentional choices—drinking water first thing in the morning, taking a short walk after lunch, pausing to breathe before eating, and winding down with a calming evening ritual. These actions, when repeated over time, create a supportive environment for the digestive system to function optimally.
The long-term benefits extend beyond physical comfort. As digestion improves, many people report increased energy, better sleep, and a greater sense of emotional balance. This is because the gut influences not only nutrient absorption and waste elimination, but also the production of neurotransmitters like serotonin, which play a role in mood regulation. When the gut is calm, the mind often follows. A lifestyle that prioritizes digestive health becomes, by extension, a lifestyle that supports overall well-being. It fosters a deeper connection between body and mind, encouraging a more compassionate and attentive relationship with oneself.
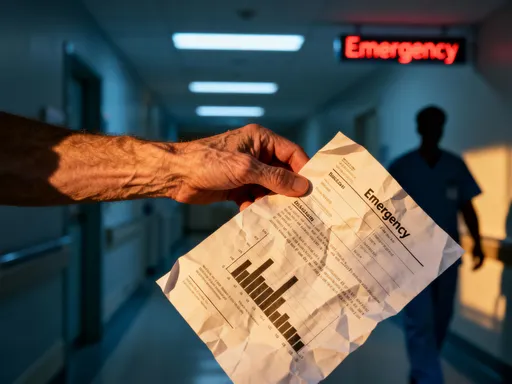
It’s important to remember that while these strategies are helpful for many, they are not a substitute for professional medical care. Persistent digestive issues, sudden changes in bowel habits, or symptoms accompanied by pain, weight loss, or fatigue should always be evaluated by a healthcare provider. Conditions such as irritable bowel syndrome, small intestinal bacterial overgrowth, or food intolerances may require specific diagnosis and treatment. The goal of this approach is not to replace medical advice, but to complement it with everyday practices that enhance the body’s natural capacity for healing and balance.